-
 chevron_right
chevron_right
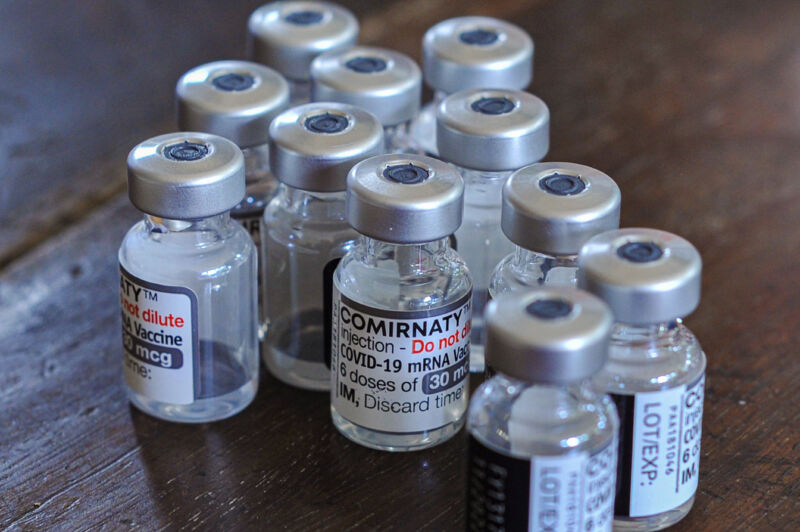
German man got 217 COVID shots over 29 months—here’s how it went
news.movim.eu / ArsTechnica · Tuesday, 5 March - 19:40

A 62-year-old man in Germany decided to get 217 COVID-19 vaccinations over the course of 29 months —for "private reasons." But, somewhat surprisingly, he doesn't seem to have suffered any ill effects from the excessive immunization, particularly weaker immune responses, according to a newly published case study in The Lancet Infectious Diseases .
The case is just one person, of course, so the findings can't be extrapolated to the general population. But, they conflict with a widely held concern among researchers that such overexposure to vaccination could lead to weaker immune responses. Some experts have raised this concern in discussions over how frequently people should get COVID-19 booster doses.
In cases of chronic exposure to a disease-causing germ, "there is an indication that certain types of immune cells, known as T-cells, then become fatigued, leading to them releasing fewer pro-inflammatory messenger substances," according to co-lead study author Kilian Schober from the Institute of Microbiology – Clinical Microbiology, Immunology and Hygiene. This, along with other effects, can lead to "immune tolerance" that leads to weaker responses that are less effective at fighting off a pathogen, Schober explained in a news release.